What is Spinal Infections and Tuberculosis?
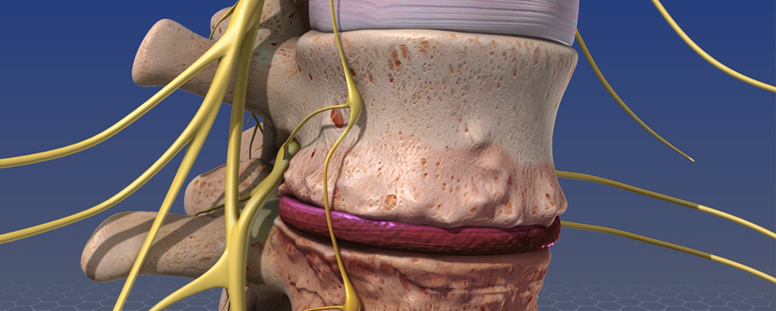
Spinal infections refer to any infection that affects the structures of the spine, including the vertebrae, intervertebral discs, spinal cord, or surrounding soft tissues. Spinal infections can be caused by bacteria, fungi, or viruses, but the most serious and globally prevalent type is spinal tuberculosis, also known as Pott’s disease. Tuberculosis (TB) of the spine is a form of extrapulmonary tuberculosis that primarily affects the vertebrae. It can cause progressive destruction of the spine, leading to deformity, instability, and neurological complications such as paralysis. Spinal infections, especially TB, can be challenging to diagnose early because symptoms develop slowly over time and are often non-specific. If left untreated, they can result in permanent damage to the spine and surrounding nerves. The incidence of spinal tuberculosis is higher in regions where TB is endemic, but it can also occur in immunocompromised individuals or those with poor access to healthcare. Prompt diagnosis and treatment with antibiotics or antifungal medications are essential to prevent long-term complications.
What are the major types of Spinal Infections and Tuberculosis?
Spinal infections and tuberculosis can be classified into several types based on the anatomical structures involved. The major types include:
- Vertebral Osteomyelitis
- Discitis
- Spinal Epidural Abscess
- Spinal Tuberculosis (Pott's Disease)
- Fungal Infections of the Spine
Explain their types
Vertebral Osteomyelitis
Vertebral osteomyelitis is an infection of the vertebral bones, often caused by bacteria such as Staphylococcus aureus. The infection typically spreads to the spine through the bloodstream from another part of the body. Symptoms include back pain, fever, and in severe cases, neurological deficits if the infection compresses the spinal cord. Diagnosis is made through imaging studies like MRI and blood tests, and treatment involves long-term antibiotics, sometimes requiring surgical intervention.
Discitis
Discitis is an infection of the intervertebral discs, which lie between the vertebrae. This condition often occurs in conjunction with osteomyelitis. It causes severe back pain, fever, and difficulty moving. Children are more prone to discitis, but it can also occur in adults, particularly after spinal surgeries or invasive procedures. Like osteomyelitis, discitis is treated with antibiotics and, in severe cases, may require surgery to stabilize the spine.
Spinal Epidural Abscess
A spinal epidural abscess is a collection of pus that forms in the space around the spinal cord or spinal nerves due to bacterial or fungal infection. It can cause significant pressure on the spinal cord, leading to pain, neurological deficits, and, if left untreated, paralysis. Symptoms include fever, severe back pain, and neurological issues like weakness or sensory changes. Prompt diagnosis and treatment with antibiotics or surgical drainage are crucial to prevent permanent damage.
Spinal Tuberculosis (Pott's Disease)
Spinal tuberculosis, also known as Pott’s disease, is a severe form of TB that affects the vertebrae. It is caused by the spread of Mycobacterium tuberculosis from the lungs to the spine via the bloodstream. This condition leads to the slow destruction of the vertebrae, often causing deformity (such as a hunched back), spinal instability, and in severe cases, neurological deficits like paralysis. Symptoms include chronic back pain, weight loss, fever, and night sweats. Treatment involves long-term antibiotic therapy and sometimes surgery to stabilize the spine.
Fungal Infections of the Spine
Fungal infections of the spine, though rare, can occur in individuals with weakened immune systems, such as those with HIV/AIDS, cancer, or those undergoing immunosuppressive therapy. Fungi such as Candida, Aspergillus, or Cryptococcus can infect the vertebrae or surrounding tissues, leading to symptoms similar to bacterial infections. These infections require antifungal medications and, in some cases, surgical intervention to remove infected tissue.
What causes a Spinal Infections and Tuberculosis?
The causes of spinal infections and tuberculosis vary depending on the type of infection. Bacterial infections, such as vertebral osteomyelitis or discitis, are often caused by bacteria entering the spine through the bloodstream from other parts of the body, such as skin infections, urinary tract infections, or pneumonia. In some cases, spinal infections may result from direct trauma or after spinal surgery. Spinal tuberculosis is caused by the Mycobacterium tuberculosis bacterium, which typically spreads from the lungs to the spine through the bloodstream. Fungal infections of the spine are usually associated with immunocompromised individuals, where the body's defenses are weakened, allowing fungal pathogens to invade the spinal structures. Risk factors for spinal infections include pre-existing conditions such as diabetes, chronic kidney disease, and HIV/AIDS. Spinal tuberculosis is more common in areas with high TB prevalence, crowded living conditions, and poor healthcare access.
Spinal Infections and Tuberculosis include:
Spinal infections and tuberculosis involve various conditions that affect different parts of the spine. These conditions include:
- Vertebral osteomyelitis
- Discitis
- Spinal epidural abscess
- Pott’s disease (spinal tuberculosis)
- Fungal infections affecting the spine
What are the symptoms of a Spinal Infections and Tuberculosis?
The symptoms of spinal infections and tuberculosis can vary depending on the type of infection and its severity. Common symptoms include:
- Persistent back pain, often worsening over time
- Fever and chills
- Night sweats (common in tuberculosis)
- Unexplained weight loss
- Weakness or numbness in the arms or legs
- Difficulty walking or maintaining balance
- Paralysis or loss of bladder/bowel control in severe cases
Risk Factors
Several risk factors can increase the likelihood of developing spinal infections or tuberculosis. These include:
- Weakened immune system (due to HIV, cancer, or immunosuppressive therapy)
- Chronic conditions such as diabetes or kidney disease
- Poor nutritional status, which weakens the body's defenses
- Living in areas with high TB prevalence
- History of intravenous drug use or untreated infections
- Recent spinal surgeries or invasive spinal procedures
- Head Injury Brain Tumour Complex Skull Base Tumours Vascular Neurosurgery Minimally Invasive Brain Surgeries Minimally Invasive Spine Surgery (MISS) Spinal Tumours Craniovertebral Junction (CVJ) Anomaly Spine Trauma Spinal Infections and Tuberculosis Neuro Intervention Endoscopic spine and Brain surgery