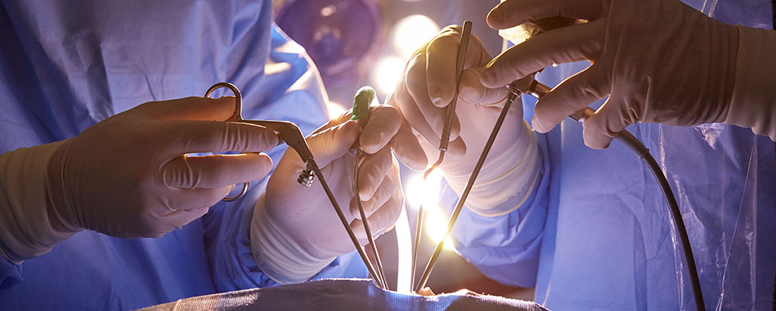
What is Minimally Invasive Brain Surgeries?
Minimally Invasive Brain Surgery (MIBS) refers to advanced surgical techniques used to treat brain disorders with smaller incisions, minimal disruption to surrounding tissue, and faster recovery times compared to traditional open brain surgery. These surgeries rely on high-tech tools such as endoscopes, microscopes, and image-guided systems to access the brain through small openings, reducing trauma to the brain and surrounding structures. The goal of MIBS is to achieve the same or better results as traditional surgery while minimizing risks such as infection, scarring, and postoperative recovery time. Surgeons performing minimally invasive brain surgery use cutting-edge imaging technologies, like MRI and CT scans, to map out the brain's intricate structures before and during the procedure. This enables more precise targeting of the affected areas, often allowing patients to resume normal activities sooner. Conditions treated with MIBS range from brain tumors and aneurysms to epilepsy and Parkinson's disease, with a growing list of applications as techniques continue to evolve.
What are the major types of Minimally Invasive Brain Surgeries?
Minimally Invasive Brain Surgery covers a range of techniques designed to treat different brain conditions with minimal harm to the patient. The major types of minimally invasive brain surgeries include:
- Endoscopic Brain Surgery
- Neuroendoscopy for Skull Base Tumors
- Stereotactic Brain Surgery
- Keyhole Craniotomy
- Laser Ablation Surgery
- Endovascular Neurosurgery
Explain their types
Endoscopic Brain Surgery
Endoscopic brain surgery involves using a thin, flexible tube called an endoscope that is equipped with a camera and light. The surgeon inserts the endoscope through small incisions in the skull or nasal cavity, allowing them to see inside the brain on a screen while operating. This approach is commonly used to treat hydrocephalus, pituitary tumors, and skull base tumors, with minimal damage to healthy brain tissue.
Neuroendoscopy for Skull Base Tumors
Neuroendoscopy is a minimally invasive technique used to remove tumors located at the skull base, such as meningiomas or chordomas. The endoscope is inserted through the nose or mouth to access these deep-seated tumors, eliminating the need for large incisions in the skull. This method reduces recovery time and minimizes complications like infection or scarring.
Stereotactic Brain Surgery
Stereotactic brain surgery uses a computer-guided system to precisely target areas within the brain based on three-dimensional imaging from MRI or CT scans. This technique is used to perform biopsies, treat brain tumors, and manage conditions like epilepsy or Parkinson’s disease. The accuracy of stereotactic surgery minimizes damage to surrounding brain tissue.
Keyhole Craniotomy
Keyhole craniotomy involves creating a small incision, usually behind the ear or in the eyebrow region, to access specific areas of the brain. This procedure is used to remove tumors, address aneurysms, or treat conditions like trigeminal neuralgia. The "keyhole" approach limits the size of the incision, reducing recovery time and scarring.
Laser Ablation Surgery
Laser ablation surgery, also known as laser interstitial thermal therapy (LITT), uses laser energy to precisely target and destroy abnormal brain tissue, such as tumors or seizure-causing areas. Guided by MRI imaging, the surgeon inserts a laser probe through a small hole in the skull and heats the affected area to remove or shrink the tissue. This method is often used for hard-to-reach tumors or intractable epilepsy.
Endovascular Neurosurgery
Endovascular neurosurgery is a minimally invasive procedure used to treat vascular disorders like aneurysms and arteriovenous malformations (AVMs) within the brain. Surgeons insert catheters into blood vessels through a small incision in the groin, guiding them to the affected area using imaging technology. The catheter delivers treatments like coils, stents, or embolic agents to block or repair damaged vessels without the need for open surgery.
What causes Minimally Invasive Brain Surgeries?
Minimally invasive brain surgery is often performed in response to medical conditions that affect the brain and central nervous system. These conditions require surgical intervention to either remove abnormal tissue, repair damaged blood vessels, or alleviate pressure within the skull. The causes that lead to minimally invasive brain surgeries include:
- Brain tumors such as meningiomas, gliomas, and pituitary tumors
- Vascular conditions like aneurysms and arteriovenous malformations (AVMs)
- Hydrocephalus (fluid buildup in the brain)
- Epilepsy requiring surgical intervention
- Trigeminal neuralgia (chronic facial pain caused by nerve compression)
- Skull base tumors that are difficult to access via traditional methods
Minimally Invasive Brain Surgeries include:
Minimally invasive brain surgeries cover a broad range of procedures that target specific brain conditions with reduced trauma to the patient. These surgeries are designed to address conditions like tumors, blood vessel malformations, and neurological disorders. Minimally invasive brain surgeries include:
- Endoscopic brain surgery
- Stereotactic brain surgery
- Neuroendoscopy
- Keyhole craniotomy
- Laser ablation surgery (LITT)
- Endovascular neurosurgery
What are the symptoms of Minimally Invasive Brain Surgeries?
Patients requiring minimally invasive brain surgery typically exhibit symptoms related to the underlying condition being treated. These symptoms may vary depending on the type of brain disorder but commonly include:
- Persistent or severe headaches
- Seizures (especially in cases of epilepsy or brain tumors)
- Vision problems such as blurred or double vision
- Hearing loss or ringing in the ears (tinnitus)
- Balance issues or difficulty walking
- Memory or cognitive impairment
- Facial pain or numbness
- Nausea or vomiting (associated with increased intracranial pressure)
Risk Factors
The risk factors for requiring minimally invasive brain surgery often depend on the underlying medical condition, but some common risk factors include:
- Family history of brain tumors or neurological disorders
- Genetic conditions such as neurofibromatosis or tuberous sclerosis
- High blood pressure and vascular diseases
- Smoking, which increases the risk of aneurysms and stroke
- Exposure to radiation or environmental toxins
- History of head trauma or injury
- Chronic infections or inflammation of the brain or nervous system
- Head Injury Brain Tumour Complex Skull Base Tumours Vascular Neurosurgery Minimally Invasive Brain Surgeries Minimally Invasive Spine Surgery (MISS) Spinal Tumours Craniovertebral Junction (CVJ) Anomaly Spine Trauma Spinal Infections and Tuberculosis Neuro Intervention Endoscopic spine and Brain surgery